Fracture Surgeries
What is Fracture Surgeries?
Fractures in joint replacement surgeries, commonly known as periprosthetic fractures, are breaks in the bone that occur around or near an implanted prosthetic joint such as the hip or knee. These fractures may happen intraoperatively, during the surgical preparation of bone or implant insertion, or postoperatively, often due to trauma, falls, weakened bone, or long-term implant-related stress. Risk factors include osteoporosis, poor bone quality, implant loosening, previous fractures, and technical errors during surgery. Clinically, patients usually present with sudden pain, swelling, loss of limb function, deformity, and inability to bear weight. Diagnosis relies on X-rays, sometimes supplemented by CT scans to assess fracture complexity and bone stock, and evaluation of implant stability. Treatment depends on the fracture type, implant fixation, and bone quality—ranging from non-surgical management with bracing in rare stable cases to surgical interventions like open reduction and internal fixation (ORIF) using plates, screws, or cables; revision arthroplasty with longer or specialized stems for loose implants; or bone grafting in cases of significant bone loss. Complications may include delayed or failed healing, persistent pain, infection, or further implant failure, making prevention vital through preoperative bone health optimization, careful surgical technique, fall prevention strategies, and regular follow-ups to monitor implant stability.

Dr. Rohan Bhargava
MBBS (KEM, Mumbai), MS Ortho, DNB Ortho
FNB Arthroplasty, MRCSEd.(UK) MNAMS
Fellowship in Revision Joint Replacement (Germany)
1. What Are They?
Fractures that occur around or near a prosthetic joint implant, such as in the hip, knee, shoulder, or elbow. They can:
Occur during surgery (intraoperative) when the bone is prepared or the implant is inserted.
Happen after surgery (postoperative), often due to falls, trauma, or weakening of bone around the implant.
2. Why Do They Happen?
Bone-related factors:
Osteoporosis or poor bone quality makes bones fragile.
Previous fractures or bone defects (e.g., bone cysts).
Implant-related factors:
Loosening of the implant increases stress on surrounding bone.
Long-stem implants or cemented stems may create stress risers.
Surgical factors:
Forceful insertion of implant components.
Malalignment or undersizing of implants.
Patient-related factors:
High fall risk due to age, weakness, or neurological problems.
Chronic steroid use, metabolic bone disease, or rheumatoid arthritis.
3. Classification Systems
Hip Replacements:
Vancouver Classification (most widely used): Considers fracture location, implant stability, and bone stock.
Knee Replacements:
Felix Classification: Based on fracture location (femur, tibia, patella) and stability.
Shoulder & Elbow Replacements:
Similar systems classify by bone involved, implant fixation, and displacement.
4. Clinical Presentation
Sudden sharp pain around the prosthetic joint.
Loss of function – inability to bear weight or move the limb.
Visible deformity, swelling, and bruising.
In severe cases, limb shortening or abnormal angulation.
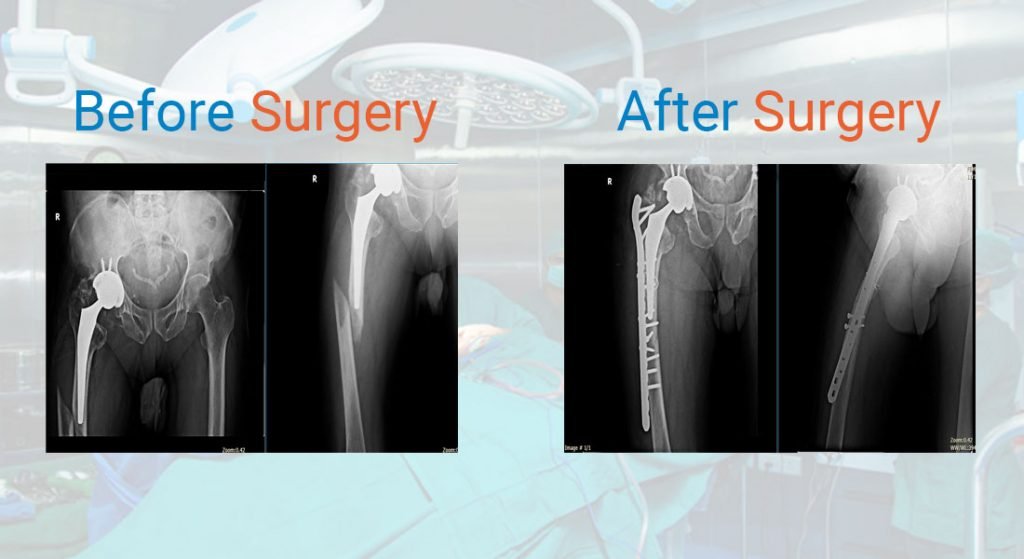
5. Diagnosis
X-rays – first-line to identify fracture type and implant position.
CT scans – to understand complex fracture patterns and bone stock.
Bone scans or nuclear imaging – if implant loosening or infection is suspected.
6. Management
Non-Surgical (rare)
Only for stable fractures with a well-fixed implant and minimal displacement.
Use of braces, casts, or restricted weight-bearing.
Surgical
Open Reduction and Internal Fixation (ORIF):
Plates, screws, and cerclage wires stabilize the fracture while preserving the implant.
Revision Arthroplasty:
Implant replaced with a longer stem or different design if loose or damaged.
Combination (ORIF + Revision):
Stabilizes fracture and replaces failing implant simultaneously.
Bone Grafting & Augmentation:
For severe bone loss, allografts or metal augments may be needed.
7. Complications
Non-union (failure of bone healing) or malunion (healing in wrong position)
Persistent pain or instability
Infection around the implant
Further implant loosening or failure
Need for additional revision surgeries
8. Prevention
Preoperative bone health optimization (treating osteoporosis).
Choosing implants that match bone quality.
Gentle surgical technique and correct sizing of implants.
Post-op physiotherapy, gait training, and fall prevention strategies.
Regular follow-up imaging to monitor implant stability.